Heavy Metals and Endocrine Disruptors
How to Avoid and Detox Them
If you’ve ever wondered why hormone problems, fatigue, brain fog, or fertility issues sometimes hang around even after you “clean up” your diet, here’s a big reason: we’re rarely exposed to one toxin at a time.
In the real world, heavy metals (like mercury, lead, cadmium, arsenic) mix with endocrine-disrupting chemicals (EDCs) such as phthalates, bisphenols (BPA/BPS), PFAS (“forever chemicals”), flame retardants and pesticides.
Those mixtures can push on the same hormone pathways at once—sometimes at very low doses—and the combined effect can be bigger than any single exposure alone.
In this guide, I’ll break down (simply and practically) how metals and EDCs interact, where they show up, how to avoid them, and how I build a gentle, structured detox plan around Dr. Georgiou’s HMD™ protocol to help the body off-load heavy metals—the part of the mixture that chelators and natural binders are actually designed to address.
Heavy metals are endocrine disruptors too
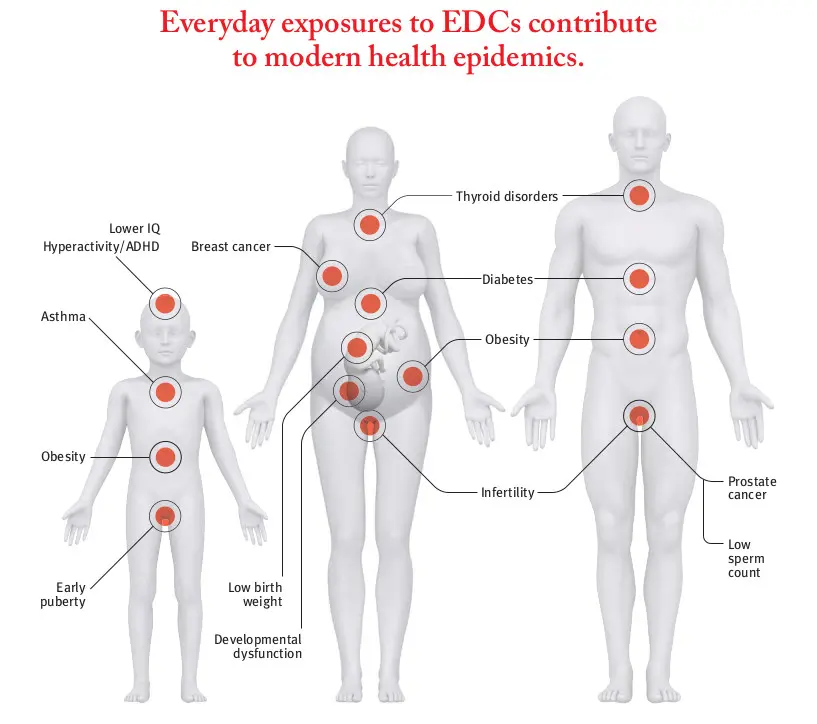
We tend to file “EDCs” under plastics and sprays, but several metals behave like hormone disruptors:
- Cadmium can act like a “metalloestrogen”, binding to estrogen receptors and mimicking estrogenic signals (the human evidence is mixed, but lab and animal data are strong).
- Lead interferes with reproduction in men and women (lower sperm quality, altered sex hormones; in women, more pregnancy complications).
- Arsenic alters glucocorticoid receptor signaling at low concentrations—one way it disrupts stress and developmental pathways.
- Mercury accumulates in the thyroid and has been linked in human studies and meta-analyses with altered TSH/T4/FT4 patterns.
The Endocrine Society’s scientific statements have repeatedly flagged endocrine disruption across thyroid, reproductive, metabolic and neuroendocrine pathways—EDCs aren’t just a laboratory curiosity. They’re relevant to real health.
Why mixtures matter: metals + EDCs push the same hormone systems
When exposures co-occur, effects can add up even if each dose is “low.” Decades of mixture research show additive or greater-than-additive effects when multiple estrogen- or thyroid-active chemicals are combined, challenging the “one-chemical-at-a-time” view of safety. Recent mixture studies also evaluate metals plus PFAS or phthalates, linking co-exposures to altered thyroid function, lipids, inflammation and reproductive outcomes.
A few real-world examples you’ll see in the literature:
- PFAS ↔ thyroid: multiple reviews and new analyses report associations between PFAS exposure and altered thyroid hormones (though strength and direction can vary by PFAS and life stage).
- Mercury ↔ thyroid: pooled human data link blood mercury to TSH/T4 shifts; mercury has also been found within human thyroid tissue.
- Phthalates ↔ reproduction & metabolism: systematic reviews associate phthalates with adverse reproductive endpoints (e.g., semen quality, fecundity) and pregnancy outcomes; oxidative stress is a likely mechanism.
Bottom line: the same endocrine axes—thyroid, estrogen/androgen, glucocorticoid and metabolic signaling—can be nudged by both metals and EDCs at once. That’s why being meticulous about exposure reduction and metal detox matters.
Where these exposures hide (quick map)
- Water: lead from aging plumbing; arsenic in some wells; PFAS in many U.S./EU supplies. Look for NSF/ANSI-certified filters (see below).
- Food: high-mercury fish (e.g., shark, swordfish, king mackerel, some tuna); rice can carry arsenic; canned foods (bisphenols in some linings); some fast-food packaging & nonstick cookware (PFAS).
- Home & products: fragranced personal care (often phthalates), stain-/water-repellent textiles and some cosmetics (PFAS), dust containing flame retardants, old paint or pottery (lead).
How I advise people to reduce daily exposure (simple and doable)
1) Filter your drinking water (the biggest win for many homes)
Choose systems certified by accredited bodies for the specific contaminant:
- Lead: look for NSF/ANSI 53 (health effects) or NSF/ANSI 58 (reverse osmosis). The EPA’s 2024/25 fact sheets show exactly what certification marks to find on packaging.
- PFAS: NSF/ANSI 53 (for specific PFAS) or NSF/ANSI 58 (RO). NSF explains PFAS reduction claims (often to <20 ppt).
Tip: certification lists are public—NSF’s database lets you check which models are actually certified for lead or PFAS (don’t rely on vague marketing).
- Rotate in low-mercury fish (e.g., wild salmon, sardines, trout).
- Cook fresh more often; limit canned foods (or choose BPA-free linings).
- Rinse rice thoroughly and cook in excess water you pour off (reduces arsenic).
- Use glass or stainless for hot foods; don’t microwave plastics (NIEHS).
- Go fragrance-free (phthalates often hide in “fragrance”/“parfum”).
- Avoid “stain-resistant,” “water-repellent,” and some nonstick coatings unless PFAS-free is clearly stated (EPA + consumer guides).
- Vacuum and damp-dust regularly to lower dust-borne EDCs and metals (NIEHS).
Detox basics that actually help (without magical thinking)
Before we talk chelation, the foundations matter—because metals and many EDCs re-circulate between liver, bile and gut:
- Fiber (25–35 g/day): binds bile and interrupts enterohepatic recirculation so more contaminants exit in stool.
- Sweating (sauna or exercise): a systematic review found arsenic, cadmium, lead and mercury can be excreted in sweat.
- Microbiome support: fermented foods and targeted probiotics can bind and transform some metals in the gut, decreasing absorption (a human probiotic yogurt pilot reported lower metal exposure markers).
- Minerals & antioxidants: selenium, zinc, magnesium and N-acetylcysteine (NAC) support antioxidant defenses and glutathione pathways that shuttle metals for excretion.
These steps won’t “chelate” PFAS or most synthetic EDCs, but they reduce re-uptake, lower oxidative stress, and set the stage for metal removal—important because mixtures amplify effects.
What chelation can (and cannot) do in mixture exposures
Chelation and natural binders are for metals. They won’t clear PFAS or most plasticizers. Still, when you lower your metal load, you can lessen the combined endocrine stress since the same axes (thyroid, reproductive, metabolic) are being pushed from multiple directions. Think of it like lowering one side of the “toxic seesaw” while you’re simultaneously avoiding EDCs.
How I use Dr. Georgiou’s HMD™ protocol to detox metals (gently, in phases)
I like HMD™ because it’s designed around the mobilize → bind → drain logic and it plays nicely with a “foundations-first” approach:
What’s in HMD™?
- HMD™ (Heavy Metal Detox) liquid: a synergistic blend including Chlorella Growth Factor, Coriandrum sativum (cilantro) and a homaccord of Chlorella pyrenoidosa.
- HMD™ LAVAGE: herbal drainage support for liver, kidneys, lymph.
- HMD™ Organic Chlorella: binder in the gut to catch metals dumped into bile. Heavy Metal Detox
What the research says
Dr. Georgiou’s team reports randomized, double-blind, placebo-controlled work in 350 metal foundry workers, testing various natural substances and combinations; their publications summarize that the HMD™ blend increased urinary/fecal excretion across multiple metals under provocation testing.
Dosing (adult guidance from the official HMD™ page)
- HMD™: 45 drops, 3× daily, 10–15 minutes before meals (titrate up slowly if sensitive).
- LAVAGE: 25 drops, 3× daily (can go in the same glass as HMD™).
- HMD™ Organic Chlorella: 2 capsules (450 mg), twice daily with breakfast and dinner.
Children’s doses are weight-based (see official page).
A common plan is 90 days per cycle, with longer courses for higher burdens and periodic re-assessment—again consistent with program guidance.
My step-by-step plan for mixed exposures (what I actually do)
Phase 0 — Exposure triage (week 1)
- Water: install a certified filter (lead → NSF/ANSI 53 or 58; PFAS → 53/58); confirm certification in the NSF database.
- Food & kitchen: swap nonstick for stainless/ceramic, use glass for hot foods, prioritize low-mercury seafood.
- Products & textiles: go fragrance-free and avoid stain-resistant/PFAS-coated items.
Phase 1 — Prime (2–4+ weeks)
- Hit fiber and hydration targets, add a daily fermented food; consider a Lactobacillus/Bifidobacterium probiotic.
- Move your body and sweat (sauna or exercise) 3–5×/week if tolerated.
- Start minerals/antioxidants (selenium, zinc, magnesium; whole-food diet; consider NAC).
Why: this strengthens the gut barrier, keeps the exit ramp open, and reduces “re-absorption.”
Phase 2 — Add HMD™ (start low, go slow)
- Begin HMD™ and LAVAGE at tolerable doses (sensitive folks may start with 5–10 drops 3×/day and step up).
- Take Chlorella with meals to catch metals entering bile.
- Keep Phase 1 habits running in the background.
Phase 3 — Monitor and personalize (ongoing)
- Track sleep, energy, headaches, skin, bowels. If “detox feelings” spike, pause the mobilizer (HMD™), continue binders/drainage, then resume low and slow.
- For objective tracking, work with a clinician on periodic urinary metals (creatinine-normalized) and basic labs to confirm kidney/liver comfort. (This is standard chelation hygiene.)
What about EDCs like PFAS or phthalates? Chelators won’t generally remove them. That’s why exposure control is non-negotiable. However, by lowering metals, you reduce overall mixture pressure on endocrine targets (thyroid, reproductive axes)—a practical way to tilt the balance back in your favor while you steer clear of EDCs.
One pilot study using HMD on a small sample of phthalates and PFAS’s has shown promise in that it did chelate some of these. Also, based on anecdotal evidence, a number of women taking HMD have regulated their periods, which may be another indication that HMD is eliminating these endocrine-disrupting chemicals.
Safety notes I give every patient
- If you’re pregnant, breastfeeding, have kidney/liver disease, complex chronic illness, or take interacting meds, work with a qualified clinician.
- Don’t “stack” multiple mobilizers at aggressive doses—more is not faster or better.
- Hydration, minerals, and bowel regularity make or break comfort during detox.
The bottom line (in plain English)
- Mixtures matter: heavy metals and EDCs often hit the same hormone pathways.
- You can control exposure today (water filter, kitchen swaps, product choices).
- You can support elimination (fiber, sweating, microbiome, minerals).
- And you can reduce the metal side of the equation with a gentle, phased plan using Dr. Georgiou’s HMD™ (mobilize), HMD™ Organic Chlorella (bind), and LAVAGE (drain)—while you keep lowering plastics/PFAS/phthalates at the source. That’s how I help clients make real progress without overwhelm.
Educational only; not medical advice. Work with a qualified clinician for personalized care, especially if you are pregnant, breastfeeding, or have kidney/liver conditions.