Clinical Use of Hair Tissue Mineral Analysis Tests
In integrative and natural medicine, practitioners who work with environmental exposure and mineral balance often lean on testing to guide a plan. The most common approach I see is a before-and-after (“pre/post”) urine or stool test, sometimes paired with a provocation agent to encourage short-term mobilization.
The tricky part is that provoked urine (or stool) testing is not a “total body burden” measurement. It’s closer to a snapshot: it shows what is moving through elimination pathways over a short window of time. That can be useful information—but it comes with limitations that aren’t always explained clearly.
Why provoked urine tests can be hard to interpret
Let’s walk through a simple example. Imagine a baseline urine sample shows a mercury level of 3 (arbitrary units). After using a provocation agent, a second sample taken a day later shows 6. What does that mean?
- It suggests that some amount of mercury is stored and can be mobilized.
- It does not tell you how much is stored overall.
- It does not tell you how much is leaving through other routes (for example, biliary elimination tends to show up more in stool than urine).
Now suppose the person repeats testing 2–3 months later and sees different numbers. You might see lower baseline and lower post-provocation numbers and feel tempted to conclude, “Great—this means we eliminated 50%.” But clinically, it’s rarely that straightforward. These values can shift for lots of reasons: hydration, timing, recent exposure, how the kidneys are functioning that day, bile flow, and how strongly the body is mobilizing at that moment.
So, provocation testing often tells you that movement is happening, but it doesn’t reliably quantify how much has cleared over time.
There’s another scenario that deserves caution: if a person’s elimination capacity is sluggish, a provoked test may show only a small rise. That doesn’t automatically mean “no stored metals.” It may simply mean the body isn’t moving much into that pathway at that time. Decisions based purely on a low provocation response should always be made carefully and in context.
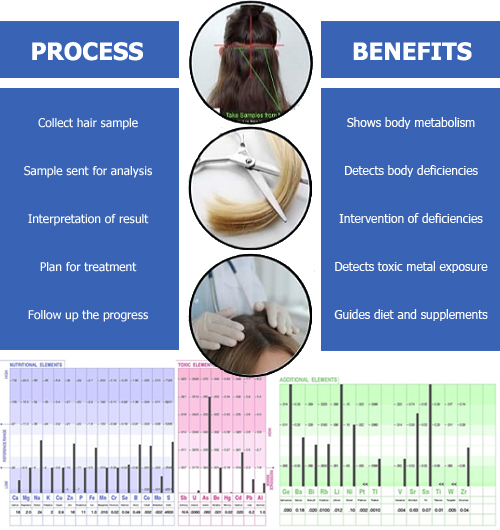
Hair Tissue Mineral Analysis (HTMA)
Because of the practical and interpretive limitations above, I often prefer Hair Tissue Mineral Analysis (HTMA) as a gentler, longer-range way to observe mineral patterns and trends. HTMA isn’t a stand-alone diagnostic tool, but when used responsibly it can add helpful context—especially when you’re tracking change over time rather than trying to capture a single 24-hour moment.
Why I find HTMA useful (when used properly)
- Gentler monitoring approach: HTMA does not require aggressive short-term mobilization, which can be a better fit for people who prefer a steadier pace.
- Trend tracking over time: Hair reflects mineral deposition over a longer window (often discussed as roughly 6–10 weeks depending on hair growth), making it easier to observe direction across repeated tests.
- Cost and convenience: A hair sample is simple to collect, and compliance tends to be much better than a 24-hour collection.
- Broader mineral context: HTMA typically reports essential minerals alongside certain metals, which can support more balanced decisions around nutrition and mineral support.
- Sample stability: Hair is stable and easier to store/ship than many other sample types.
- Sensitivity for detection: Because minerals can be present in higher concentrations in hair than in blood, certain patterns may be easier to notice—especially when comparing the same person across time.
Important note: HTMA can be influenced by external contamination (hair dye, swimming pools, occupational dust), so it should always be interpreted alongside history, symptoms, and good clinical judgment—not in isolation.
How I Use HTMA in Clinical Practice
Here’s a structured way HTMA can be used to guide a protocol and track trends:
- Baseline: Collect an initial hair sample and document the person’s history, possible sources of exposure, diet, mineral intake, and key symptoms.
- Begin a structured protocol: Start a consistent plan designed to support normal elimination and overall resilience. (In our clinic setting, this is where HMD® is often introduced as part of a broader approach.)
- Retest after ~8 weeks: Repeat HTMA after enough time for new hair growth to reflect that period.
- Read the pattern, not a single number: Sometimes you may see a rise in certain metals on the second test. Interpreted responsibly, this can suggest the body is expressing more through hair during the period being measured—one reason I value trend tracking rather than relying on a single “snapshot” test.
- Continue periodic monitoring: Repeating HTMA at steady intervals helps you see whether trends are moving in a favorable direction over time and supports sensible adjustments to pacing and consistency.
The goal isn’t to chase perfection or panic at one data point. The goal is to build a repeatable, steady system that lets you make practical decisions over time.
Suppose metals are present in the storage organs. In that case, the probability is that you will get a dramatic INCREASE in the toxic metals compared to baseline – this indicates that the HMD® is pulling heavy metals out of storage sites into the blood and then into the hair.
This indicates that the person has metals stored in the body, and the clinical decision is to continue taking the HMD®. Diagram 1 and Diagram 2 provide some examples of this. Diagram 1 shows a young 3-year-old boy—the left test is the baseline, and the right test is after the HMD® protocol for 2 months. There is a dramatic increase in the metal cadmium from 0.022 to 115 mg%—this was traced to the mother, who also had extremely high levels.
Diagram 1. Pre-test (left) and post-test (right) showing high level of toxic metals in a 3-year-old child, after being on the HMD™ oral chelation protocol

Diagram 2. Pre-test (left) and post-test (right) showing high level of toxic metals in a 29-year-old mail, after being on the HMD™ oral chelation protocol
Diagram 2 shows the level of mercury rising after taking the HMD® protocol for two months. The hair test can be repeated after a further two months but always while they are still taking the HMD®.
A reduction in metals shows that the person is on the right track, and the storage sites are diminishing. You can keep repeating this until there are negligible metals on the HTMA, which is a reflection of negligible metals in the body’s storage sites.
Conclusion
Used responsibly, HTMA can be a valuable way to track mineral patterns over time. It’s convenient, repeatable, and often easier to interpret as a trend tool than a single provoked urine snapshot. The most important piece is always the same: interpret results in context, move steadily, and focus on a plan that supports long-term consistency.
Educational note: This information is for general education only and is not medical advice. If you have a medical condition, are pregnant or nursing, take medication, or have concerns about exposure, work with a qualified healthcare professional before starting any new protocol.